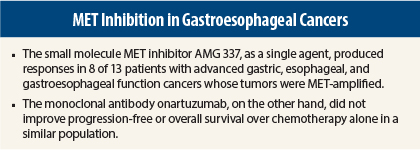
The MET pathway appears to be important in gastroesophageal cancers, but response to a targeted agent may depend on the class of drugs. A robust response to the novel small-molecule MET inhibitor AMG 337 was observed, but a monoclonal antibody targeting MET fell flat, in studies reported at the 2015 Gastrointestinal Cancers Symposium.
The MET signaling pathway is abnormal in a variety of cancers, and aberrant upregulation of MET has been associated with a poor prognosis. MET signaling stimulates cell growth, invasion, and metastasis and promotes resistance to apoptosis, making MET an attractive therapeutic target, speakers said.
Potent Tyrosine Kinase Inhibitor
Eunice Kwak, MD, PhD, of Massachusetts General Hospital in Boston, called responses to AMG 337 monotherapy “dramatic” in patients with MET-amplified gastric, esophageal, and gastroesophageal junction tumors.1
AMG 337 is a potent and highly selective inhibitor of wild-type and some mutated forms of MET. In laboratory studies, cancer cells showing MET gene amplification demonstrated sensitivity to the drug, whereas other cells appeared insensitive.
The dose escalation and dose expansion study reported by Dr. Kwak included 90 patients with a variety of advanced solid tumors, who had received a median of two prior lines of therapy. Of this population, 21 had gastric, esophageal, or gastroesophageal junction tumors. Of the 90 patients overall, MET gene amplification was observed in 19 patients (21%).
Outcomes ‘Dramatic’ in MET-Amplified Subset
Of the 21 patients with gastric, esophageal, or gastroesophageal junction tumors, 13 have been treated to date. Of this subset, all of whom had MET-amplified tumors, eight patients responded, for an objective response rate of 62% to single-agent treatment, Dr. Kwak reported, labeling this a “dramatic” response to a single agent.
Four patients are still on active treatment; one of these patients has responded for 96 weeks, and another has responded for 155 weeks.
Among the 90 patients in the entire population, grade ≥ 3 adverse events were reported in 21%, primarily headache (7.8%). About 50% of patients had headaches of varying degrees of severity.
Dr. Kwak emphasized the importance of MET amplification in the population. “All of the patients who achieved a response had some sort of MET abnormality in their tumors,” she said. “This demonstrates that MET is an oncogenic driver in some of these cancers.”
MET amplification could prove to be a useful biomarker, she said. “If we have robust biomarkers that tell us we have cancers that are being driven by specific signals, it can change the way we think about treating patients, with the goal being that we can make huge—or at least larger—impacts on patient survival,” she pointed out.
The daily maximum tolerated dose has been set at 300 mg, and a twice-daily maximum tolerated dose is still being determined. A dose expansion phase will enroll up to 50 patients with MET-amplified tumors at the maximum tolerated dose. A phase II study of AMG 337 in patients with MET-amplified gastroesophageal junction, gastric, or esophageal cancer or other MET-amplified solid tumors is currently recruiting patients.
Monoclonal Antibody Falls Flat
In contrast, the MET-inhibiting fully humanized monoclonal antibody onartuzumab proved ineffective in a phase II study of the drug in combination with FOLFOX (fluorouracil/leucovorin/oxaliplatin) in patients with advanced gastroesophageal adenocarcinoma. MET positivity was defined as ≥ 50% moderate-to-high staining for MET by immunohistochemistry.2
“The addition of onartuzumab to modified FOLFOX6 in metastatic gastroesophageal adenocarcinoma did not improve progression-free survival in either an unselected population or in patients with MET-positive tumors, as defined by immunohistochemistry,” said Manish Shah, MD, of NewYork-Presbyterian Hospital, New York.
In the multicenter study presented by Dr. Shah, 123 patients with metastatic HER2-negative gastroesophageal adenocarcinoma received FOLFOX alone or with onartuzumab (10 mg/kg every 2 weeks) for 12 cycles, followed by onartuzumab monotherapy until disease progression. The primary endpoint was progression-free survival.
In the intent-to-treat population, median progression-free survival was 6.77 months in the onartuzumab arm and 6.97 months with FOLFOX alone (hazard ratio [HR] = 1.06, P = .7149). In the MET-amplified population, median progression-free survival was 5.95 and 6.8 months, respectively (HR = 1.38, P = .4514). The stratified HR for progression-free survival in the MET-negative population was 0.99, Dr. Shah reported.
In an exploratory analysis by strength of MET staining, “There was no clear signal that very high MET staining altered survival” with respect to onartuzumab benefit, he said.
At the time of data cutoff, only 50% of patients had died. Median overall survival was approximately 11 months in each arm in the intent-to-treat population and approximately 8.5 months in the MET-positive population.
Onartuzumab-specific toxicity included edema and venous thromboembolism.
“The question now is how to identify MET-driven tumors? Is it immunohistochemistry, amplification, or something else?” Dr. Shah suggested. “That’s the main question with MET inhibition moving forward.” ■
Disclosure: Dr. Kwak has received research funding from Amgen (via her institution). Dr. Shah has a consulting or advisory role with Lilly and Sanofi-Aventis and has received research funding from Bayer/Onyx, Genentech, and Sanofi-Aventis (all via his institution).
References
1. Kwak EL, LoRusso P, Hamid O, et al: Clinical activity of AMG 337, an oral MET kinase inhibitor, in adult patients with MET-amplified gastroesophageal junction, gastric, or esophageal cancer. 2015 Gastrointestinal Cancers Symposium. Abstract 1. Presented January 15, 2015.
2. Shah MA, Cho JY, Huat ITB, et al: Randomized phase II study of FOLFOX +/- MET inhibitor, onartuzumab, in advanced gastroesophageal adenocarcinoma. 2015 Gastrointestinal Cancers Symposium. Abstract 2. Presented January 15, 2015.