Improved relapse-free survival following treatment with adjuvant trastuzumab (Herceptin) appears to be associated with a heightened state of immunologic function, according to genomic analysis that resulted in a 14-gene profile predictive of outcomes in the landmark NCCTG (Alliance) N9831 trial.1
“We have identified a predictive model for adjuvant trastuzumab, using an approach that integrates genomics, biology, and clinical outcome data. This genomic analysis reveals a major immunologic component that is predictive of the clinical benefit of adjuvant trastuzumab,” said Edith A. Perez, MD, Deputy Director at Large at the Mayo Clinic Cancer Center, Jacksonville, Florida, and the principal investigator of N9831, which helped establish the benefit of adjuvant trastuzumab.
The findings suggest that breast cancer could join the ever-growing list of malignancies that might be subject to immune modulation.
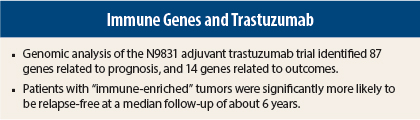
“We are very enthusiastic about the results,” Dr. Perez told The ASCO Post. “We validated the findings with 100 replications, and they all led to the same 14-gene panel, with all genes associated with immune function. Our work has taken 4 years. It is very solid. We have a prognostic panel of 87 genes and a 14-gene predictive panel.”
At the 2014 ASCO Annual Meeting, Dr. Perez presented the findings of a genomic analysis of N9831 tissue samples. The study’s aim, she said, was to identify biologic principles that underlie the clinical outcomes of early-stage HER2-positive breast cancer. To this end, her team developed, evaluated, and validated a multigene predictive signature for response to adjuvant trastuzumab.
Genomic Analysis
The investigatgors used Illumina’s 24K DASL whole-transcriptome technology to quantify mRNA abundance in 1,282 tumor samples. They identified 473 genes in the chemotherapy-alone arm associated with recurrence-free survival and 510 in the trastuzumab/chemotherapy combined arms, independent of nodal status, tumor size, hormone receptor status, age, and tumor grade. Using the genes that were significantly associated with outcome, they used pathway enrichment statistics to assess the biologic significance of four functional “interactome” models.
In the trastuzumab-treated patients, six biologic pathways were associated with increased relapse-free survival. These pertained to cytokine-cytokine receptor interaction, T-cell receptor signaling in CD8-positive T-cells, the interferon-gamma pathway, tumor necrosis factor receptor signaling pathway, cell surface interaction at the vascular endothelium, and class 1 PI3K signaling events.
“Four of these significant pathways are linked to immunologic function,” she noted. “This was the first indication that there is an important immunologic component to benefit from adjuvant trastuzumab.”
Dr. Perez and her team did not stop there: They assigned each of the 510 genes a gene ontology identifier, resulting in 13 biologic process descriptors with different distribution in patients treated only with chemotherapy, compared with those also receiving trastuzumab. Of these, 10 descriptors were associated with increased relapse-free survival. These 10 processes defined a cohort of 87 immune function genes.
“These 87 genes were prognostic for outcomes in patients who got chemotherapy plus trastuzumab,” she said. Of these 87 genes, 14 demonstrated a significant interaction with trastuzumab treatment vs chemotherapy alone, and these formed the predictive gene signature.
“Our interest went beyond identifying a prognostic signature. We wanted to identify a predictive signature. Of the 87 genes, we found 14 that had significant interaction P values (P < .05) in the trastuzumab arms vs the nontrastuzumab arms,” Dr. Perez said. “These 14 genes were integrated into a voting scheme model that predicts trastuzumab response.”
The model labels patients as “immune-response enriched” or not and predicts for trastuzumab response, independent of nodal or hormone receptor status. About 50% of both the trastuzumab-treated and chemotherapy-alone cohorts in the N9831 sample had immune-response enriched tumors.
Immune-Enriched Patients
Most importantly, patients with immune-enriched tumors experienced a favorable outcome when treated with trastuzumab. “We found that immune enrichment predicts response to trastuzumab,” Dr. Perez reported.
Among immune-enriched patients, the hazard ratio (HR) for relapse-free survival for those receiving trastuzumab was 0.36 (P < .0001), compared with chemotherapy treatment alone. When tumors were not immune-enriched, trastuzumab conferred no benefit over chemotherapy alone (HR = 0.99, P = .91). “Those curves were the same,” she observed. “For those not enriched, there were no differences in relapse-free survival whether they received adjuvant trastuzumab or not.”
To confirm that this 14-gene signature was generalizable, the investigators conducted a fivefold cross-validation and repeated it 100 times. “In each of the 100 tests, we got the same data, showing that patients whose tumors were immune-enriched did the best when receiving chemotherapy plus trastuzumab vs all the other patients and tumors.”
“This observation may define a significant biologic process that is linked to the efficacy of HER2-targeted therapy, may provide a means of predicting probability of relapse following adjuvant trastuzumab, and suggests possible routes of therapeutic enhancement,” she said.
“We feel there are significant implications for our 14-gene predictive immune signature,” she said at the ASCO session. “It can help us evaluate and understand the mechanisms of sensitivity and resistance to trastuzumab and it has potential implications for enrollment criteria in future clinical trials.”
Dr. Perez suggested that patients presumed to be HER2-negative by central testing but who respond to trastuzumab may be responsive because they express these immune-related genes. ■
Disclosure: Dr. Perez reported no potential conflicts of interest. For full disclosures of all study authors, visit abstracts.asco.org.
Reference
1. Perez EA, et al: Association of genomic analysis of immune function genes and clinical outcome in the NCCTG (Alliance) N9831 adjuvant trastuzumab trial. ASCO Annual Meeting. Abstract 509. Presented May 31, 2014.