Bilateral prophylactic mastectomy may ease cancer-related anxiety for patients at high risk of breast cancer, but it does very little to contain the costs. A study presented at the American Society of Breast Surgeons 16th Annual Meeting found that bilateral prophylactic mastectomy was not cost-effective unless the patient has a lifetime breast cancer risk of about 50%.1 The typical woman’s lifetime risk is 12%, although factors such as family history, certain benign breast conditions, and hormone use can elevate this risk.
“Cost-effectiveness analysis is an increasingly important tool to aid in clinical decision-making, particularly in today’s age of health-care reform,” said Brandy Edwards, MD, a general surgery resident at the University of Virginia, Charlottesville, who led the study.
“Previous studies have made the economic case for prophylactic procedures in women with BRCA mutations or contralateral mastectomies for patients with cancer in the other breast. This is the first study to demonstrate that a woman without breast cancer or known genetic mutation must have substantial risk to cost-justify prophylactic surgery.”
Study Details
The study was an overview of cost-effectiveness studies that examined screening and prevention in high-risk women, in terms of life-years or quality-adjusted life-years gained, which represent a year of life in perfect health. It showed that annual screening mammography is significantly more cost-effective than bilateral prophylactic mastectomy in managing the care of most women at high risk for breast cancer. Women with a known BRCA gene mutation, which carries an exceptionally high risk, as well as women with multiple concomitant risk factors are a notable exception.
The study relied on a Markov model, which simulates effects that change over time. Model parameters included costs, sensitivity, and specificity of screening modalities, as well as mortality rates. Incremental cost-effectiveness ratios were calculated and interpreted with respect to willingness-to-pay thresholds—typically $50,000 and $100,000. The study assumed a 90% breast cancer risk reduction with bilateral prophylactic mastectomy. It focused on patients beginning at age 30 and assumed that full lifetime risk would be met at age 80.
“Based on information in published literature, we also adjusted the model to account for expected patient preferences for [bilateral prophylactic mastectomy] compared to screening,” noted Dr. Edwards.
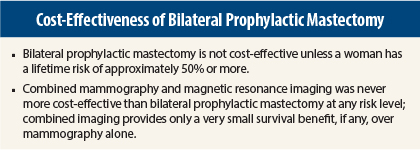
Even in this subset, the numbers showed that bilateral prophylactic mastectomy should primarily be considered only in women with a very high risk. When accounting for these patient preferences, an approximate 50% lifetime risk still emerged as the point where bilateral prophylactic mastectomy would be considered a cost-effective alternative to screening, she reported.
The study also found that screening with a combination of mammography and magnetic resonance imaging (based on Medicare reimbursement rates) was never more cost-effective than bilateral prophylactic mastectomy at any risk level and that the additional survival benefit associated with combined screening is very small, if any, when compared to mammography screening alone.
Lifetime Risk Must Be Substantial
The key numbers from the analysis—for the cost-effectiveness of bilateral prophylactic mastectomy—were as follows:
- At a willingness-to-pay threshold of $50,000, in unadjusted life-years gained, the lifetime risk must be at least 43%; in quality-adjusted life-years, the risk must be at least 57%.
- At a willingness-to-pay threshold of $100,000, in unadjusted life-years gained, the lifetime risk must be at least 26%; in quality-adjusted life-years, the risk must be at least 51%.
“Our model suggests that [bilateral prophylactic mastectomy] should primarily be considered in women with a substantial risk of breast cancer,” Dr. Edwards concluded.
However, while cost-effectiveness studies are a valuable tool for comparing interventions, she said the results should not be the sole criterion for deciding whether or not a certain treatment should be used or covered by health insurance.
“At the end of the day, this is a highly personal decision that must be made on a patient-by-patient basis,” she said.
“Clearly there is a need for additional affordable screening technologies for women at high risk for breast cancer,” Dr. Edwards added. “While prophylactic mastectomy is appropriate for some women, it can carry steep costs, both economically and in quality-of-life, because prophylactic surgery isn’t without risk.” ■
Disclosure: Dr. Edwards reported no potential conflicts of interest.
Reference
1. Edwards BL, Hu Y, Stukenborg GJ, et al: Cost-effectiveness of bilateral prophylactic mastectomy in patients at high risk for breast cancer without known BRCA mutation. American Society of Breast Surgeons Annual Meeting. Presented April 30, 2015.