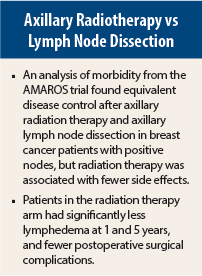
Radiation therapy is associated with significantly fewer postoperative complications than axillary lymph node dissection, according to a detailed analysis of morbidity from the AMAROS (After Mapping of the Axilla: Radiotherapy or Surgery?) trial presented at a press briefing prior to the American Society of Breast Surgeons (ASBS) Annual Meeting in Las Vegas.
Previous reports from this trial have shown no difference in survival among women receiving either treatment, but results from this international prospective multicenter trial suggest that radiation therapy has the advantage of producing fewer side effects, said Mila Donker, MD, of the Netherlands Cancer Institute and Antoni van Leeuwenhoek Hospital in Amsterdam.
“Surgical complications [in patients receiving radiotherapy] were more than twice as high for patients having lymph node dissection [vs axillary radiotherapy] and the rate of lymphedema at 5 years was also twice as high,” Dr. Donker reported.
The AMAROS trial of 4,806 early-stage breast cancer patients randomly assigned those with positive sentinel nodes (n = 1,425) to treatment with axillary lymph node dissection (n = 744) or axillary radiotherapy (n = 681), including the medial part of the supraclavicular fossa. At the ASBS meeting, investigators presented the analysis of morbidity, including the predictive value of treatment factors.
Surgical Complications
Patients receiving axillary dissection had an overall surgical complication rate of 22.6% vs 9.0% for the axillary radiotherapy group (P < .001). This included higher rates of hemorrhage, postoperative infections, and other conditions.
Lymphedema at 1 year post-treatment was observed in 25% and 15%, respectively (P < .001), and in 59% of the 27 patients who received both axillary lymph node dissection plus axillary radiotherapy (P < .001 vs axillary radiotherapy). After 5 years, the rates of lymphedema were 21%, 10%, and 58%, respectively (P < .001 vs axillary radiotherapy).
The independent risk factors for the development of lymphedema within the first year were treatment with axillary lymph node dissection, which carried more than twice the risk vs axillary radiotherapy, or treatment with the combination, where the risk was more than sevenfold; a body mass index > 25 kg/m2, premenopausal status, and treatment on the dominant side also raised the risk for lymphedema. Paresthesia of the arm was observed in 10% after axillary lymph node dissection and 9% after axillary radiotherapy.
Shoulder mobility decreased temporarily, particularly during the first year in both treatment arms. Risk factors for shoulder problems at 1 year included treatment with axillary lymph node dissection (as compared to axillary radiotherapy), the addition of isolated supraclavicular radiotherapy after axillary lymph node dissection, and more extensive axillary lymph node dissection.
“Our morbidity data strongly support radiotherapy as the preferred treatment,” Dr. Donker concluded.
Deanna J. Attai, MD, of the Center for Breast Care in Burbank, California, who moderated the press briefing, commented, “We have been performing fewer axillary dissections as there is a growing body of literature demonstrating no local recurrence or survival benefit as well as an increased rate of complications. However, there are still patients for whom an axillary dissection may be indicated. This study demonstrates that we do have alternatives for reducing local recurrence rates and can safely avoid surgery and the associated complications in some patients.” ■
Disclosure: Drs. Donker and Attai reported no potential conflicts of interest.
Reference
1. Donker M, Rutgers E, van de Velde C, et al: Axillary lymph node dissection vs axillary radiotherapy: A detailed analysis of morbidity. ASBS Annual Meeting. Presented April 30, 2014.