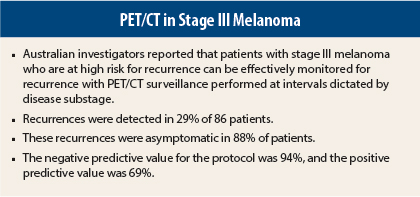
In monitoring patients with melanoma at high risk for relapse, surveillance imaging with 18F-fluorodeoxyglucose–positron-emission tomography (FDG-PET)/computed tomography (CT) can detect asymptomatic metastases and thus facilitate early treatment, according to Australian investigators who presented their findings at the 2015 ASCO Annual Meeting.1 Jeremy Lewin, MBBS, of the Peter MacCallum Cancer Centre, East Melbourne, Victoria, Australia, presented the study, which sought to determine if PET/CT can accurately detect early recurrences and thus facilitate earlier treatment.
Benefits and Risks
“Many benefits and risks are associated with radiologic surveillance of stage III melanoma,” Dr. Lewin noted. “Among the benefits are the ability to identify treatable locoregional recurrences with the hope of allowing access to early surgical resection or effective new systemic treatments. There is also the reassurance associated with negative scans,” he said.
Potential risks include false-positives, cumulative radiation exposure, increased cost of care, inconvenience to patients, and psychological distress in anticipation of the scans, he said.
Dr. Lewin noted that relapse in stage III melanoma is not homogeneous but is dependent upon substage and may be curable in many cases. The optimal surveillance strategy remains unclear and is often done at the discretion of the treating physician, he indicated.
“Given the increasing sensitivity of FDG-PET in identifying metastatic disease, we have been conducting substage-specific radiologic surveillance in stage III patients, in hopes of identifying increased asymptomatic relapses,” he said.
Study Details
Since 2009, patients at the Peter MacCallum Cancer Centre with fully resected stage III melanoma have undergone such surveillance. This retrospective analysis included 86 patients who had whole-body PET/CT scans, performed according to their estimated substage relapse probabilities. PET/CT scans were performed as follows:
- Stage IIIA: 6, 18 months (n = 11)
- Stage IIIB: 6, 12, 18, 24, 36, 48, 60 months (n = 50)
- Stage IIIC: 6, 12, 18, 24, 36 months (n = 25), including MRI of brain at 6 and 12 months
This resulted in a total of 232 PET/CT scans. Relapse was suspected in 35 patients (41%); in this group, 25 relapses were confirmed, and 10 patients were determined to be disease-free. Confirmed relapses, therefore, were observed in 29% of the total scanned group, including 1 of 11 stage IIIA patients (9%), 15 of 50 stage IIIB patients (28%), and 10 of 25 stage IIIC patients (40%).
“Of the 25 relapses, 22 (88%) were asymptomatic at the time of scanning,” Dr. Lewin reported. “First relapses in stage IIIA/B patients were more likely than stage IIIC to be locoregional.”
Among stage IIIA and stage IIIB patients, 40% of relapses were locoregional, whereas 60% were metastatic. Among stage IIIC patients, only 10% were locoregional, whereas 90% were metastatic.
Nine relapsed patients (36%) were able to undergo potentially curative resection, including one stage IIIA patient, six stage IIIB patients, and two stage IIIC patients; five of them (all stage IIIA/B) were free of disease after a median of 32 months’ follow-up after nodal resection.
Most relapsed patients who were unable to have surgery did receive systemic therapy, including ipilimumab (Yervoy), BRAF inhibition, radiotherapy, and chemotherapy.
Incidental findings were detected 24 times in 19 patients (22%). This included 6 patients with a new diagnosis of a different malignancy; all received treatment, most with curative intent. A number of patients had other incidental, nonmalignant findings necessitating medical workup
Sensitivity and Specificity
“We found a favorable sensitivity and specificity of substage-specific PET/CT after resected stage III melanoma,” Dr. Lewin reported.
By the gold standard of histologically confirmed relapse during the surveillance period, the protocol had a sensitivity of 88% and a specificity of 84%. Based on a prevalence of 29%, the negative predictive value was 94%, though the positive predictive value was only 69%, he indicated.
Negative predictive value was also very high when analyzed per-scan and per-patient. Per-scan, the negative predictive value was 99% for stage IIIB and 97% for stage IIIC patients, and per-patient negative predictive value was 97% and 86%, respectively. The positive predictive value per-scan was 69% and 73%, respectively, and per-patient positive predictive value was 68% and 73%, respectively.
“The high [negative predictive value] provides reassurance,” Dr. Lewin commented. ■
Disclosure: Dr. Lewin reported no potential conflicts of interest.
Reference
1. Lewin J, Sanelli A, Walpole I, et al: Surveillance imaging with FDG-PET in the follow-up of melanoma patients at high risk of relapse. 2015 ASCO Annual Meeting. Abstract 9003. Presented May 30, 2015.