Patients with stage IV pancreatic cancer who received a novel enzyme along with standard chemotherapy experienced a doubling in progression-free survival, compared to those given chemotherapy alone, in a study presented at the 2015 ASCO Annual Meeting.1 Response rates and median duration of response were also doubled, and a trend toward improved survival was observed as well, reported Sunil R. Hingorani, MD, PhD, of Fred Hutchinson Cancer Research Center, Seattle.
“Collectively, these data have prompted the planning of a global phase III trial,” Dr. Hingorani indicated.
Study 202
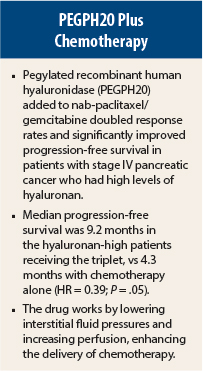
Dr. Hingorani presented interim results from a randomized, multicenter phase II trial testing a novel combination therapy dubbed PAG—pegylated recombinant human hyaluronidase (PEGPH20) plus nab-paclitaxel (Abraxane) and gemcitabine—in patients with stage IV pancreatic cancer.
Poor outcomes in pancreatic cancer are associated in part with tumor stroma that limits chemotherapy perfusion. These tumors express high levels of hyaluronan, which has a number of detrimental effects on the tumor and microenvironment. PEGPH20 depletes hyaluronan in tumors, he explained.
The ongoing phase II Study 202 has a target enrollment of 260 patients. It had enrolled 146 patients between March 2013 and April 2014, before a clinical hold was placed on the study after a higher thromboembolic event rate was observed in the PEGPH20 arm compared with the control arm. At that time, the 29 patients still receiving PEGPH20 were maintained on nab-paclitaxel/gemcitabine alone.
At the time of the clinical hold, 28.4% of the PAG arm and 14.8% of the chemotherapy-alone arm had experienced a thromboembolic event, mainly pulmonary embolism, deep-vein thrombosis, and in a few patients, arterial events. As a result, the protocol was amended to exclude patients with a history of or increased risk for thromboembolic events, and patients in both arms were given low–molecular-weight heparin as prophylaxis.
Dr. Hingorani presented the efficacy and safety data for patients enrolled up to the clinical hold and the thromboembolic rates after institution of the protocol amendment. He reported on 135 patients with a median follow-up of 7 months. Of the 135 patients, 106 were able to be evaluated for hyaluronan expression and were classified as hyaluronan-high or hyaluronan-low.
Hyaluronan Expression
“In these overall populations, the suggestion of improved efficacy did not reach statistical significance. However, when patients were stratified by [hyaluronan] content, there were two observations,” he reported.
In hyaluronan-low patients, there appeared to be no benefit to adding PEGPH20, “which might be expected, if hyaluronan is a specific target,” he pointed out. In contrast, in the hyaluronan-high patients, the results were striking.
In the hyaluronan-high subset, the overall response rate was 52% in the PAG arm, compared to 24% with chemotherapy alone (P = .038), and median duration of response was 8.1 months vs 3.7 months, respectively. Restricting the evaluation to patients treated before the clinical hold (and therefore not contaminated by crossover), the investigators observed an even larger difference, with response rates of 73% and 27%, respectively (P = .01).
Median progression-free survival was 9.2 months in the hyaluronan-high patients receiving PAG, vs 4.3 months with chemotherapy alone (hazard ratio [HR] = 0.39; P = .05). Again, no differences were observed in the hyaluronan-low subset.
“A trend in overall survival in the triplet arm reflected the differences noted by the other measures and does include data on 12 of the 23 PAG patients who discontinued the enzyme and got nab-paclitaxel/gemcitabine alone, after the hold,” Dr. Hingorani said. Median overall survival was 12 months with PAG and 9 months with chemotherapy alone (HR = 0.62).
Thromboembolic Events
Treatment-related adverse events seen more frequently with PAG included peripheral edema (58% vs 31%), muscle spasms (55% vs 2%), and neutropenia (32% vs 18%).
After initiation of prophylaxis with enoxaparin at 40 mg/d, the rate of thromboembolic events “normalized” between the arms, at approximately 29% for both groups. For patients initiated on enoxaparin at 1 mg/kg/d, the risk of thromboembolic events was ameliorated even further, to 0% with PAG and 10% with nab-paclitaxel and gemcitabine. These findings suggest that the thromboembolic risk can be adequately managed, he said. ■
Disclosure: Dr. Hingorani is a consultant for Halozyme Therapeutics.
Reference
1. Hingorani SR, Harris WP, Hendifar AE, et al: High response rate and PFs with PEGPH20 to nab-paclitaxel/gemcitabine in stage IV previously untreated pancreatic cancer patients with high-HA tumors: Interim results of a randomized phase II study. 2015 ASCO Annual Meeting. Abstract 4006. Presented May 31, 2015.