
We know that metastatic breast cancer survival is much better now than 20 years ago, but we also know there’s a role for surgery of the primary tumor.— Atilla Soran, MD, MPH
Tweet this quote
For de novo stage IV breast cancer, does resection of the primary tumor improve outcomes? Two studies presented at the 2016 ASCO Annual Meeting reached different conclusions. A prospective randomized study conducted in Turkey concluded there is a survival benefit at 5 years,1 whereas a U.S. registry–based study showed a lack of benefit.2 Both assessed the effect of resection of the primary tumor on overall survival in women presenting with stage IV disease.
Key Findings of Both Studies
Atilla Soran, MD, MPH, a Turkish-born surgical oncologist who practices at the Magee-Womens Hospital of the University of Pittsburgh Medical Center, presented the results of the MF07-01 trial sponsored by the Turkish Federation of Breast Diseases Societies.1
“In the first 3 years, we found that survival was similar for surgery and no surgery, but longer follow-up revealed a significant improvement of about 9 months in median overall survival. Five-year overall survival was 42% with surgery, vs 25% with systemic therapy alone,” revealed Dr. Soran.
The greatest benefit was observed in patients with estrogen receptor–positive, HER2-negative disease, patients with solitary bone metastases, and those younger than age 55—“persons with a more indolent form of metastatic breast cancer,” he added. On the other hand, patients with multiple liver and/or pulmonary metastases had a significantly worse prognosis with initial surgery.

In the absence of prospective data, our findings do not support surgery for the primary tumor outside of a clinical trial.— Tari King, MD
Tweet this quote
The U.S.-based TBCRC 013 trial was presented by Tari King, MD, on behalf of the Translational Breast Cancer Research Consortium (TBCRC).2 This prospective registry study was initiated in 2009—a time when retrospective data suggested a survival benefit for surgery, but prospective data did not, she explained.
“The role of surgery in the management of de novo stage IV breast cancer remains controversial…. Prior to the latest analysis of the Turkish study, the prospective data that were available to date did not support an overall survival benefit,” she said. “We designed a registry with the goal of characterizing patients presenting with stage IV breast cancer in the modern era while capturing their clinical management and outcomes,” Dr. King reported.
The researchers found 3-year overall survival to be 70%. The majority of patients (85%) responded to first-line therapy, and response was significantly associated with overall survival. Among responders, 30-month survival was 76% without surgery and 77% with surgery. Among nonresponders (who did not receive surgery), it was 13 months, with 30-month survival being 24%.
“This was a registry study, so patients selected for surgery were more likely to have single-organ metastatic disease and to have received first-line chemotherapy. Yet despite the selection bias, surgery did not impact overall survival in any tumor subtype,” Dr. King revealed. “In the absence of prospective data, our findings do not support surgery for the primary tumor outside of a clinical trial,” she concluded.
Turkish Study Details
The Turkish study included 274 women who presented with stage IV breast cancer. Based on the extent of disease, patients received surgery followed average 4 weeks later by systemic therapy (n = 138) or systemic therapy alone (n = 136). Surgery was a breast-conserving approach (with whole-breast radiotherapy) or mastectomy (with or without radiotherapy, based on the extent of disease and institutional practice). Patients with positive nodes received axillary clearance, and hormonal therapy and/or trastuzumab (Herceptin) was given if indicated.
Baseline characteristics were similar between the groups. Most patients had grade 2–3 T2 or T3 invasive ductal carcinoma. Approximately 30% of each arm had HER2-positive disease. The surgery group had more hormone receptor–positive disease (86%) than did the systemic therapy group (73%) and less triple-negative disease (7% vs 17%). Approximately 50% of patients had bone-only metastases.
Turkish Study: Survival Benefit
At 3 years, overall survival was 68% with surgery and 51% with systemic therapy, which was not significantly different (P = .10); however, differences emerged by 5 years, where 41.6% of the surgery group was alive, compared with 24.4% of the systemic therapy group (hazard ratio [HR] = 0.66; P = .005). Median overall survival at that time was 46 months and 37 months, respectively.
“Surgery prolonged median overall survival by about 9 months,” Dr. Soran said. A post hoc subgroup analysis revealed subsets of patients who appeared to derive the most benefit from surgery (Table 1).
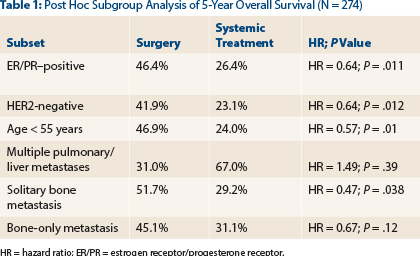
Surgery added an additional 7 months for estrogen receptor/progesterone receptor–positive patients, 12 months for HER2-negative patients, 14 months for patients < 55 years old, 10 months for patients with a solitary bone metastasis, and 14 months for patients with bone-only metastases (the difference in the bone-only group was not significant). In addition, locoregional relapse was 11 times less with surgery, 1% vs 11%. When censored for early relapse, surgery still provided a 39% reduction in relapse, he added.
“We know that metastatic breast cancer survival is much better now than 20 years ago, but we also know there’s a role for surgery of the primary tumor,” Dr. Soran concluded. He added that performance status, age, comorbidities, and burden of metastatic disease should be factors in considering surgery and that surgical benefit depends on “the completeness of resection” and the use of axillary surgery and locoregional radiotherapy.
U.S. Study Details
A body of retrospective data has suggested “a consistent survival benefit for the use of surgery” in stage IV de novo disease, at least in the setting of multimodality care and especially among patients with estrogen receptor/progesterone receptor–positive cancers, according to Dr. King, but more studies were deemed warranted to settle this question. Six prospective randomized trials attempted to do so; three have required patients to receive systemic treatment before being randomized to surgery or not, whereas the other three studies, including the Turkish study, randomized patients to surgery or no surgery prior to receipt of systemic therapy.
The U.S. study included 112 patients with an intact primary tumor, enrolled between 2009 and 2012 at 14 institutions. After first-line therapy per treating physician, responders could consider elective surgery, the type and extent of which was by physician discretion.
Median age was 51 years, median tumor size was 3.2 cm, and most patients had estrogen receptor/progesterone receptor–positive and some had HER2-negative disease. Bone-only disease was recorded for 46%, and single-organ metastatic disease was observed in 57%.
U.S. Study: Lack of Survival Benefit
At a median follow-up of 54 months, the 3-year overall survival was 70%, and median survival was 69 months. A total of 94 patients (85%) responded to first-line therapy (and then could have surgery or not), whereas 17 patients (15%) did not respond.
To correct for potential bias in comparing survival between responders and nonresponders, the researchers performed a landmark analysis, which measured survival only among patients surviving to 6 months—a point that was considered a surrogate for response to systemic therapy. “It was clear that patients who respond to first-line therapy achieve significantly improved survival over those who do not,” stated Dr. King. Median survival was 65 months among responders, with a 30-month survival rate of 78%, compared with only 13 months for nonresponders, and a 30-month survival rate of 24% (P < .001).
Among the 94 responders, 39 proceeded with elective surgery (median time of 7 months). These patients had larger tumors and were more likely to have single-organ metastatic disease and to have had first-line chemotherapy. Other factors were not different between the groups.
Surgery and Survival in Stage IV Breast Cancer
- Two studies presented at the 2016 ASCO Annual Meeting reached different conclusions about the benefit of surgical resection of the primary tumor in stage IV de novo metastatic breast cancer.
- In a randomized prospective Turkish study of 274 women, median overall survival at 5 years was 46 months and 37 months, respectively, for a 9-month overall advantage.
- Conversely, in the U.S.-based registry study of 112 women, median overall survival was approximately 70 months, with no differences in the arms.
In the multivariable analysis, when censored for survival at 6 months, surgery of the primary did not improve overall survival among responders, who had a median survival of 71 months, vs 65 months without surgery. This finding translated to 30-month survival rates of 77% and 76%, respectively (P = .85).
The comparable survival held true for the estrogen receptor and HER2 subgroups. When the results were further broken down into combinations of estrogen receptor and HER2 status, she added, “we were unable to find a subgroup where surgery improved survival,” though they were very small subsets. Among responders, HER2 status and patient age remained strong prognostic factors. An exploratory analysis of estrogen receptor–positive, HER2-negative patients with results from the 21-gene recurrence score also showed no survival benefit with the use of surgery in the various risk categories. ■
Disclosure: Dr. Soran has consulted for NanoVision Diagnostics. Dr. King reported no potential conflicts of interest.
References


