The homologous recombination deficiency (HRD) score may be a predictive biomarker of response to neoadjuvant platinum-based therapy in patients with triple-negative breast cancer, according to studies presented at the 2015 San Antonio Breast Cancer Symposium.
“We found, in our adjusted analysis, that patients with [homologous recombination]–deficient tumors were 4.6 times more likely to achieve a pathologic complete response,” said Melinda L. Telli, MD, of Stanford University School of Medicine, Palo Alto, California.
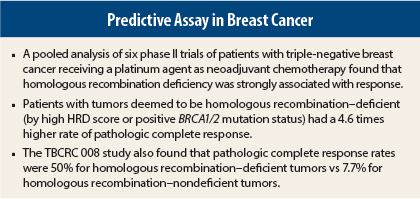
Dr. Telli presented findings from a pooled analysis of six phase II trials in which patients with triple-negative breast cancer received a platinum agent.1 Homologous recombination deficiency status was significantly associated with an improved odds of achieving a pathologic complete response (ypT0/is ypN0), regardless of BRCA1/2 mutation status.
HRD Assay
Homologous recombination–deficient tumors have lost the ability to repair double-stranded DNA breaks, resulting in increased susceptibility to DNA-damaging drugs such as platinum agents and PARP (poly ADP-ribose polymerase) inhibitors. Genomic instability and a high frequency of BRCA1 and BRCA2 germline mutations are commonly associated with triple-negative breast cancer.
Myriad Genetics has developed an HRD assay that generates an HRD score and assesses BRCA1 and BRCA2 in the tumor. The test, which may become available this year for ovarian cancer, is a next-generation sequencing assay that uses DNA extracted from formalin-fixed paraffin-embedded or frozen tumor tissue. The test labels a tumor homologous recombination–deficient or –nondeficient by combining the HRD score that it generates and the BRCA1/2 mutation status of the tumor. In short, this deficiency corresponds to an HRD score ≥ 42 and/or a mutation in BRCA1/2.
“What this test gives you is a readout of how genetically unstable the genome is,” Dr. Telli told The ASCO Post. The goal is to have an assay that can identify patients without BRCA mutations who might have a good chance of responding to DNA-damaging therapies, such as platinum, she explained.
Details of Pooled Analysis
A total of 267 patients with triple-negative breast cancer and known HRD status were analyzed from the following clinical trials: GeparSixto (n =101), PrECOG 0105 (N = 72), NCT00580333 (N = 32), NCT01372579 (N = 26), NCT00148694 (N = 18), and TBCRC 008 (N = 18).
Neoadjuvant chemotherapy regimens in the respective trials included (1) paclitaxel, nonpegylated liposomal doxorubicin, carboplatin, and bevacizumab (Avastin); (2) carboplatin, gemcitabine, and iniparib; (3) cisplatin and bevacizumab; (4) cisplatin; (5) carboplatin plus eribulin (Halaven); and (6) and carboplatin and nanoparticle albumin-bound (nab) paclitaxel (Abraxane), with or without vorinostat (Zolinza).
The primary endpoint was correlation of pathologic complete response and homologous recombination deficiency status. Secondary analyses correlated pathologic complete response and a binary HRD score (< 42 [low] vs ≥ 42 [high]) as well as pathologic complete response and homologous recombination deficiency in the BRCA1/2-negative subgroup.
Response Rates
In the pooled analysis, 178 (67%) patients had homologous recombination–deficient tumors, 89 (33%) had homologous recombination–nondeficient tumors, and 106 (39.7%) had tumors that had a high HRD score but were BRCA-negative.
A pathologic complete response was achieved in 41% of all patients. Patients with triple-negative breast cancer with homologous recombination–deficient tumors were significantly more likely to achieve a pathologic complete response than those with homologous recombination–nondeficient tumors: 53% vs 18% (adjusted odds ratio = 4.64; P < .0001), Dr. Telli reported.
In patients who were BRCA-negative but had a high HRD score, 50% achieved a pathologic complete response. This group had 4.5 times greater odds of achieving pathologic complete response than BRCA-negative patients who were homologous recombination–nondeficient (P < .0001).
Associations between response and stage, age, and planned duration of therapy were not statistically significant.
Findings From TBCRC 008
Although HRD has been investigated in triple-negative breast cancer and BRCA-associated breast cancers, it has not been studied in hormone receptor–positive breast cancer. Researchers from the TBCRC 008 trial reported the results of an exploratory biomarker study correlating baseline HRD status with pathologic complete response in patients with HER2-negative breast cancer treated with neoadjuvant therapy including a platinum, regardless of estrogen receptor status.3
HRD status and pathologic complete response data were available for 48 of the 62 patients from the study, including 30 who were hormone receptor–positive and 18 with triple-negative breast cancer. Of these patients, 46% were homologous recombination–deficient, including 33% of the hormone receptor–positive tumors and 67% of the triple-negative breast cancer tumors.
“This is the first study to look at a hormone receptor–positive cohort treated with a platinum,” declared
Roisin M. Connolly, MB, BCh, of Johns Hopkins School of Medicine, Baltimore, who presented the poster at the 2015 San Antonio Breast Cancer Symposium.
The results of the exploratory analysis support prior observations that HRD status is a promising potential predictive biomarker of response to platinum agents in triple-negative breast cancer, Dr. Connolly added.
“We observed a significantly higher pathologic complete response rate in patients with homologous recombination deficiency, vs no deficiency (50% vs 7.7%; P = .002). In the hormone receptor–positive and triple-negative breast cancer subgroups, we did see an increase in pathologic complete response with homologous recombination deficiency, but these values were not statistically significant; they were trends,” she said.
Within the subset without BRCA mutations, a significantly higher pathologic complete response rate was observed in those with high vs low HRD scores (64.3% vs 7.7%; P < .001).
“Further evaluations are warranted in both triple-negative breast cancer and estrogen receptor–positive breast cancer to help determine if the predictive effect is restricted to platinum-based chemotherapy,” Dr. Connolly said. ■
Disclosure: Dr. Telli reported no potential conflicts of interest. Dr. Connolly has received research funding for clinical trials from Genentech, Clovis, Novartis, Merrimack, Puma Biotechnology.
References
1. Telli ML, et al: Homologous recombination deficiency (HRD) as a predictive biomarker of response to neoadjuvant platinum-based therapy in patients with triple negative breast cancer. 2015 San Antonio Breast Cancer Symposium. Abstract P3-07-12. Presented December 10, 2015.
2. Connolly R, et al: Homologous recombination deficiency as a predictive biomarker of response to preoperative systemic therapy in TBCRC 008 comprising a platinum in HER2-negative primary operable breast cancer. 2015 San Antonio Breast Cancer Symposium. Abstract P3-07-13. Presented December 10, 2015.
3. Connolly RM, et al: TBCRC 008: Early change in 18F-FDG uptake on PET predicts response to preoperative systemic therapy in human epidermal growth factor receptor 2-negative primary operable breast cancer. J Nucl Med 56:31-37, 2015.