In a study that reflected clinical practice, treatment of diffuse large B-cell lymphoma based on the results of interim positron-emission tomography (PET) was feasible; however, switching PET-positive patients to an alternative treatment still resulted in inferior treatment outcomes, and the majority did not achieve a negative PET scan, according to Canadian researchers. Laurie H. Sehn, MD, MPH, Clinical Associate Professor at the British Columbia Cancer Agency and the University of British Columbia, Vancouver, and colleagues presented the results of their phase II trial at the 56th American Society of Hematology (ASH) Annual Meeting and Exposition in San Francisco.1
“Patients who were PET-negative following four cycles of R-CHOP [rituximab (Rituxan), cyclophosphamide, doxorubicin, vincristine, prednisone] had an excellent outcome, without needing radiotherapy. PET-positive patients had a poorer outcome but did better than expected compared to historical reports. However, relatively few PET-positive patients converted to a negative PET scan following R-ICE [rituximab, ifosfamide, carboplatin, etoposide], suggesting that simply switching to this alternate non–cross-resistant chemotherapy regimen is insufficient to overcome the inherent resistance in this poor-risk population,” Dr. Sehn said.
Need to Optimize Initial Therapy
“While the majority of patients with advanced-stage [diffuse large B-cell lymphoma] will be cured with R-CHOP, those [in whom front-line therapy fails] continue to have a dismal outcome,” she noted. “Optimization of initial therapy remains an important goal.”
Interim PET scanning is prognostic in diffuse large B-cell lymphoma and may enable treatment to be tailored, as it could identify patients for whom R-CHOP is insufficient. For patients with positive interim PET scans, alternate non–cross-resistant therapies could be considered prior to the emergence of further drug resistance.
With this rationale, a phase II trial was initiated to assess the feasibility and efficacy of PET-tailored therapy for diffuse large B-cell lymphoma in British Columbia. The study enrolled 155 patients (median age, 53) between October 2006 and May 2014 (stage III/IV or stage I/II with B symptoms or bulky mass ≥ 10 cm).
Patients were treated with standard-dose 3-weekly R-CHOP and could be enrolled at any time prior to cycle 4 without need for a staging PET scan. Interim PET scans were performed at a centralized site following cycle 4. Those with a negative PET scan received two additional cycles of R-CHOP, whereas patients with a positive PET scan were switched to receive four cycles of R-ICE and had a final PET scan after treatment completion.
“As per the policy in British Columbia, patients with a positive PET post-treatment received consolidative radiation therapy, if feasible, and this was not considered to be an event with respect to progression-free survival,” Dr. Sehn indicated. Patients with an indeterminate PET were recommended to complete treatment with R-CHOP. Patients with disease progression during cycles 1 to 4 of R-CHOP were taken off study.
Key Data
Of the 150 evaluable patients who underwent interim PET scanning, 88 (59%) were PET-negative, 50 (33%) were PET-positive, and 12 (8%) were PET-indeterminate. PET-positive patients were more likely to have elevated LDH and bulky disease at diagnosis.
All PET-negative patients completed treatment with R-CHOP as intended, and none received radiotherapy. Of the 50 PET-positive patients, 2 refused to switch to R-ICE and completed treatment with R-CHOP (both received radiotherapy), whereas 48 proceeded to R-ICE. Of these 48, 9 patients failed to complete all four cycles of R-ICE due to toxicity, and 6 of the 9 switched back to R-CHOP; 3 had disease progression during R-ICE and did not have a final PET scan.
The remaining 36 of the 50 PET-positive patients completed four cycles of R‑ICE and underwent a final PET scan. This revealed that 11 had a negative PET post R-ICE (2 received radiotherapy, regardless), whereas 25 had a positive PET post R-ICE (12 received radiotherapy). Of the 12 PET-indeterminate patients, 10 completed treatment with R-CHOP (one received radiotherapy), and 2 were switched to R-ICE (without radiotherapy).
Survival Outcomes
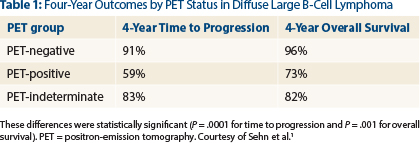
With a median follow-up of 45 months, the 4-year progression-free survival of the entire evaluable cohort was 79% and the overall survival was 87%, Dr. Sehn reported. “Overall survival was extremely favorable for PET-negative patients. PET-positive patients had a less favorable outcome but did better than expected compared to historical controls. PET-indeterminate patients had an intermediate outcome,” she noted (Table 1).
While PET-tailored therapy in patients with advanced-stage diffuse large B-cell lymphoma was feasible in this population, switching to R-ICE was fairly toxic, Dr. Sehn indicated. Nine of 48 patients (19%) were unable to complete the planned four cycles due to toxicity, which included poor tolerance (n = 5), cytopenias/infection (n = 2), allergy (n = 1), and neurotoxicity (n = 1). Intolerability did not correlate with older age; the average age of these 9 patients was 43 years.
“PET-positive patients are a group for whom novel treatments should be explored,” Dr. Sehn suggested. ■
Disclosure: Dr. Sehn has received honoraria for consultancy from Roche/Genentech, Gilead, Lundbeck, Janssen, Amgen, Celgene, and Seattle Genetics and research funding from Roche/Genentech. For complete disclosures of all study authors, see the abstract at www.hematology.org.
Reference
1. Sehn LH, et al: Phase 2 trial of interim PET scan-tailored therapy in patients with advanced stage diffuse large B-cell lymphoma in British Columbia. 2014 ASH Annual Meeting. Abstract 392. Presented December 8, 2014.