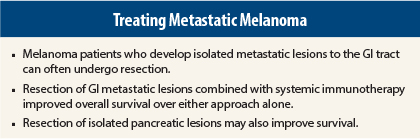
When melanoma patients develop metastases to the gastrointestinal (GI) tract or pancreas, resection of these lesions may improve survival, according to two single-institution studies presented at the 2015 Gastrointestinal Cancers Symposium. In a study that earned a Merit Award, researchers reported that resection of GI metastatic lesions combined with systemic immunotherapy improved overall survival over either approach alone.1
“Treatment of GI melanoma metastases should include a combination of metastasectomy and immunotherapy,” said Gary Deutsch, MD, MPH, of the John Wayne Cancer Institute at Providence–St. John’s Health Center, Santa Monica, California. “And the ability to achieve a surgical cure results in a superior melanoma-specific survival, compared to palliative surgery.”
The study reported by Dr. Deutsch, involving 457 patients, appears to be the largest series of GI tract melanoma metastases reported to date. The aim of the study was to clarify the role of surgical resection in the setting of systemic immunotherapy.
“Our question was how to best manage melanoma patients who develop GI metastases, which are quite common. Traditionally, systemic treatment options were not very good for metastatic disease, and we were very aggressive with resecting isolated lesions,” he said. “That used to be the best we could offer these patients, but we actually achieved long-term survival in up to 15% of patients.”
The availability of better systemic therapy—specifically ipilimumab (Yervoy) and anti–[programmed cell death 1 (PD-1)] agents—might enhance the effect of surgery when used in combination, the researchers postulated.
Dr. Deutsch said he often sees patients who have disease progression on treatment with ipilimumab, which renders them ineligible to continue on a clinical trial of that agent. “They come to us, and we look at it from a systemic perspective,” he said. “They may have one small metastasis that is growing, which we can take out. Maybe it’s a resistant clone that is not responding to ipilimumab, and we can render them NED [no evidence of disease]…. We wanted to evaluate the subset of such patients with GI tract metastases.”
Study Details
The study was a review of 457 melanoma patients who developed GI tract metastases between 1971 and 2013. Median time from initial diagnosis to the identification of GI metastasis was 49.5 months. Of the 457 patients, 270 (59%) had undergone surgical resection of GI metastases; 308 (67%) had been treated with immunotherapy.
The primary endpoint of the analysis was melanoma-specific survival after diagnosis of the GI metastases. The Kaplan-Meier analysis compared immunotherapy alone (ipilimumab, vaccine, interleukin-2 [Proleukin], interferon), surgery alone, combination therapy, and neither approach in a multivariable analysis. Patients who underwent surgery were further stratified by surgical intent.
Survival Advantage
A statistically significant survival advantage was observed for patients who were treated with both surgery and immunotherapy. Median overall survival was 20 months for this group, compared to 13 months with surgery alone, 8 months with immunotherapy alone, and only 5 months when neither treatment was delivered (P < .01).
When surgery was performed with curative intent, the outcomes were even better, with median survival being 30 months, vs 12 months when surgery was palliative (P = .02).
The group receiving surgery plus immunotherapy did not significantly differ in terms of patient and tumor characteristics from the group undergoing surgery alone, so patient selection did not appear to strongly influence these findings, he said.
On the multivariable analysis, factors significantly associated with survival included metastasectomy (hazard ratio [HR] = 0.54, P < .01), immunotherapy (HR = 0.68, P = .03), age at GI metastasis diagnosis (HR = 1.01, P < .01), and primary tumor location on the trunk vs head and neck; (HR = 1.66, P = .02).
“Younger patients with longer median time from their primary diagnosis to GI metastasis were more often selected for surgical treatment,” he noted.
Dr. Deutsch predicted that with increasing use of anti–PD-1 agents, “the survival differences may be even more pronounced.”
In an interview with The ASCO Post, Dr. Deutsch indicated, “We are trying to change the treatment paradigm for metastatic disease. I think the combination approach is where we are headed, which will be even more exciting in the future, when we have both ipilimumab and the PD-1 inhibitors available, and potentially even newer, more effective agents.”
“I think surgery will have a role in two ways,” he continued. “One is where patients treated with immunotherapy do not have a good response. I think there may be a role for aggressive surgical resection in selected patients. Secondly, and more interestingly, is in situations where patients respond to immunotherapy except for one or two isolated sites. If we address these surgically, the two approaches can potentially be synergistic.”
Pancreatic Metastasectomy Improves Survival
Similarly, in a study considered the largest series of its kind, researchers from Moffitt Cancer Center, Tampa, Florida, reported outcomes for melanoma patients who underwent resection of lesions isolated to the pancreas.2 This situation rarely occurs; therefore, this “large” series included only 24 patients, who underwent potentially curative resection between 1998 and 2013.
The 5-year overall survival rate was 67% and 5-year disease-specific survival rate was 67%. Of the 24 patients, 10 died of their disease.
These outcomes for disease-free interval and overall survival were comparable to those observed after resection of the more common metastases from renal cell carcinoma. The overall survival rate was higher than the previously reported 5-year survival of 27%, according to lead author Matthew P. Doepker,
MD, of Moffitt Cancer Center, who suggested, “Pancreatic metastasectomy for melanoma should be considered in select patients with isolated metastases,” he said. ■
Disclosure: Drs. Deutsch and Doepker reported no potential conflicts of interest.
References
1. Deutsch GB, Kirchoff D, Bailey M, et al: Gastrointestinal metastases from melanoma. 2015 Gastrointestinal Cancers Symposium. Abstract 340. Presented January 16, 2015.
2. Doepker MP, Juan TH, Chen DT, et al: Association of pancreatic metastasectomy for melanoma with long-term overall survival. 2015 Gastrointestinal Cancers Symposium. Abstract 264. Presented January 16, 2015.