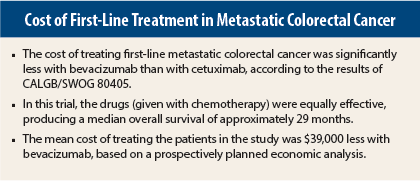
The landmark CALGB/SWOG 80405 trial concluded that bevacizumab (Avastin) and cetuximab (Erbitux) provide comparable benefit in the treatment of metastatic colorectal cancer. However, in terms of cost, bevacizumab was recently declared the winner. In an economic analysis presented at the 2015 ASCO Annual Meeting, researchers reported that treatment with bevacizumab cost $39,000 less per patient than cetuximab.1
“Chemotherapy plus bevacizumab costs less and achieves very similar survival and quality-adjusted survival as chemotherapy plus cetuximab for first-line treatment of KRAS wild-type metastatic colorectal cancer,” announced Deborah Schrag, MD, MPH, of Dana-Farber Cancer Institute, Boston.
The results of the CALGB/SWOG 80405 head-to-head comparison of the drugs were presented at the 2014 ASCO Plenary Session last year by Venook and colleagues.2 At a median follow-up of 24 months, median overall survival was 29 months in the bevacizumab arm and 29.9 months in the cetuximab arm, and median progression-free survival was 10.8 months and 10.4 months, respectively.
From Clinical to Cost Findings
The current analysis evaluated the regimens in terms of their cost-effectiveness, an analysis that was prospectively planned for CALGB/SWOG 80405, “given the high costs of all the study arms,” Dr. Schrag said.
For the average patient, the 2014 cost for one 8-week cycle of treatment was $9,324 for bevacizumab and $20,856 for cetuximab. This was based on an average selling price of $66.6 per 10 mg of bevacizumab, given at 5 mg/kg every 2 weeks, for a total of 1,400 mg, and $53.3 per 10 mg of cetuximab, given at 250 mg/m2 every 2 weeks (400 mg/m2 for the first dose), for a total of 3,913 mg for an 8-week cycle.
The two strategies were analyzed for incremental cost-effectiveness and cost-utility ratios, taking into account a number of measures. These included the utilization and cost of chemotherapy with either FOLFOX (folinic acid, fluorouracil, oxaliplatin) or FOLFIRI (folinic acid, fluorouracil, irinotecan), similar costs for end-of-life care, post-progression treatment, hospitalizations, genomic testing, and chair time, and major care episodes related to treatment.
Dr. Schrag and colleagues determined that not only were the regimens equally efficacious, they were also similar in terms of quality-adjusted life years (QALYs). Life-years and QALYs hovered around the 3.00 mark for all health outcome measurements on the EQ-5D instrument. The only difference in a subjective measurement was greater “skin satisfaction” with bevacizumab.
One Drug Just Costs More
The sizable difference in cost between the treatment arms largely stemmed from the difference in the cost of the two biologics. The analysts figured that the cost difference would neutralize if the average selling price of cetuximab was reduced by 45%.
Dr. Schrag said the findings have influenced her practice. “There’s a good argument” for using bevacizumab first-line, she said. “That’s what I do.” ■
Disclosure: Dr. Schrag reported no potential conflicts of interest.
References
1. Schrag D, Dueck AC, Naughton MJ, et al: Cost of chemotherapy for metastatic colorectal cancer with either bevacizumab or cetuximab. 2015 ASCO Annual Meeting. Abstract 6504. Presented May 30, 2015.
2. Venook AP, Niedzwiecki D, Lenz HJ, et al: CALGB/SWOG 80405: Phase III trial of irinotecan/5-FU/leucovorin or oxaliplatin/5-FU/leucovorin with bevacizumab or cetuximab for patients with KRAS wild-type untreated metastatic adenocarcinoma of the colon or rectum. 2014 ASCO Annual Meeting. Abstract LBA3. Presented June 1, 2014.