Emerging effective treatment options for salvage therapy in Hodgkin lymphoma were described by Anas Younes, MD, Chief of the Lymphoma Service at Memorial Sloan Kettering Cancer Center, New York, at the 2014 Highlights of ASH in North America meeting in Miami.
“This is an exciting time in Hodgkin lymphoma. New agents appear promising, and based on mature results of clinical trials, we may be able to reduce our patients’ exposure to potentially toxic therapy and improve outcomes in challenging patients, such as the elderly,” Dr. Younes said.
Brentuximab Vedotin After Autologous Transplant
Three-year follow-up data from a recently completed multicenter phase II trial of brentuximab vedotin (Adcetris) in patients with relapsed or refractory Hodgkin lymphoma after autologous transplant were presented at the 2013 American Society of Hematology (ASH) Annual Meeting by Ajay K. Gopal, MD, of University of Washington/Fred Hutchinson Cancer Research Center, Seattle, and colleagues.1 The drug contains a potent antitubulin agent (monomethyl auristatin E), a protease-cleavable linker, and an anti-CD30 monoclonal antibody.
The study involved 102 patients with relapsed or refractory Hodgkin lymphoma after autologous stem cell transplant, treated with brentuximab vedotin at 1.8 mg/kg every 3 weeks for up to 16 cycles.
In this high-risk population known to have a poor prognosis, the median time to relapse after autologous transplant was 6.7 months. Patients received a median of nine cycles of brentuximab vedotin, which led to an overall response rate of 75%, with complete remissions achieved in 33% of these patients.
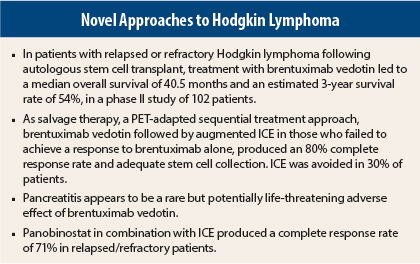
The patients were analyzed approximately 3 years after their first dose of brentuximab vedotin. Of the 102 patients enrolled, 51 (50%) were still alive, yielding a median overall survival of 40.5 months and estimated 3-year survival rate of 54%. Median progression-free survival by central independent review was 9.0 months for patients achieving a complete or partial response and only 2.8 months for those with stable or progressive disease.
“The long-term follow-up of complete and partial responses shows that 25% or so continue to be in remission, and this is remarkable,” Dr. Younas commented.
The most common grade 3/4 adverse events were neuropathy (9% grade 3) and neutropenia (14% grade 3, 6% grade 4).
“This brings us to the ongoing debate about the optimal treatment for patients failing autotransplant and now achieving a complete response with brentuximab. Should we send them immediately to allogeneic transplant, or wait? It seems that patients can remain in complete remission for several years,” he noted.
“My personal preference for patients achieving a rapid complete response with brentuximab is to wait,” he said. “Why? The toxicity associated with allogeneic stem cell transplant in this setting remains fairly high, and its efficacy in Hodgkin lymphoma is not as good as it is with other lymphoid malignancies. Furthermore, the data suggest we can re-treat with brentuximab and achieve a second response, and then do an allogeneic transplant.”
Brentuximab, ICE in Sequence
Pretransplant 18F-fluorodeoxyglucose–positron-emission tomography (FDG-PET) normalization is the strongest predictor of outcome after autologous transplant for patients with relapsed or refractory disease. Alison J. Moskowitz, MD, of Memorial Sloan Kettering Cancer Center, and colleagues used a PET-adapted sequential treatment approach with brentuximab vedotin and augmented ICE (ifosfamide, carboplatin, etoposide) prior to autotransplant as salvage therapy.2
The phase II study included 40 patients with relapsed/refractory disease who experienced treatment failure on one prior regimen. Patients received weekly brentuximab vedotin at 1.2 mg/kg for 3 weeks on, 1 week off, for two cycles followed by PET. Patients whose PET normalized proceeded to autologous transplant, while those remaining PET-positive received two cycles of augmented ICE prior to being considered for transplant.
PET-adapted sequential salvage therapy with brentuximab vedotin followed by augmented ICE produced an 80% complete response rate and an adequate stem cell collection, and it facilitated the referral to autologous stem cell transplant for virtually all patients, the authors reported.
“With this approach, 30% of patients avoided ICE salvage therapy,” Dr. Younes noted. Of 40 evaluable patients, 36 completed transplant, 3 will undergo transplant shortly, and 1 remains on treatment for persistent disease. The study was amended for an additional 20 patients, who will receive three cycles of brentuximab vedotin prior to the first PET (before ICE).
Pancreatitis as a Side Effect of Brentuximab
Pancreatitis was reported to be an adverse event of brentuximab vedotin treatment in a study by Mitul Gandhi, MD, of Robert H. Lurie Comprehensive Cancer Center, Feinberg School of Medicine, Northwestern University, Chicago, and colleagues reported at the ASH Annual Meeting.3
“Pancreatitis is a previously unidentified, rare (< 1%) but potentially life-threatening toxicity of brentuximab,” Dr. Younes said.
The study described one index case and eight additional cases of pancreatitis in patients receiving the drug, two of which were fatal. The index patient was a 65-year-old with no conventional risk factors for pancreatitis. She received two cycles of brentuximab vedotin prior to AVD and developed grade 3 diarrhea and abdominal pain after the first dose. Nine days after the second dose, she was hospitalized with acute, severe pancreatitis. She died 6 days later of sepsis and multisystem organ failure.
The autopsy specimen demonstrated fat necrosis and coagulation necrosis of the pancreas, with CD30 positivity found in 35% of analyzed cells, “which was surprising,” Dr. Younes noted. An analysis of the eight additional cases indicated the condition develops early, after about two standard doses of the drug.
“Be aware of this. In patients who experience abdominal pain following treatment with brentuximab, especially during the first few cycles, stop the treatment and investigate for pancreatitis. The good news is, it’s very rare,” he said.
Panobinostat for Hodgkin Lymphoma
The potent oral histone deacetylase inhibitor panobinostat given in combination with standard ICE led to an overall response rate of 86%, with complete responses in 15 of 21 patients (71%) in a phase I study reported by Yasuhiro Oki, MD, of The University of Texas MD Anderson Cancer Center, Houston, and colleagues.4 Panobinostat was given on Monday, Wednesday, and Friday, beginning 1 week before the first ICE treatment and continued during ICE through the second cycle. The third cycle was given without panobinostat, based on concerns over stem cell collection. The starting dose of panobinostat was 20 mg, with a target dose of 30 mg.
Of the 18 responders, 17 patients had autologous transplant without additional treatment (except for stem cell mobilization). Three patients received one or more additional treatments, then went on to transplant. There were no issues with harvest or engraftment, Dr. Younes reported.
“This is only a phase I study, but at face value the results are probably slightly better than what we expect with ICE alone,” Dr. Oki suggested. A randomized phase II study has been initiated. ■
Disclosure: Dr. Younes reported consultancy, research funding, and/or honoraria from Novartis, Seattle Genetics, Millennium, and Syndax.
References
1. Gopal AK, Chen R, Smith SE, et al: 2013 ASH Annual Meeting. Abstract 4382. Presented December 9, 2013.
2. Moskowitz A, Schoder H, Gerecitano JF, et al: 2013 ASH Annual Meeting. Abstract 2099. Presented December 7, 2013.
3. Gandhi M, Evens AM, Fenske TS, et al: 2013 ASH Annual Meeting. Abstract 4380. Presented December 9, 2013.
4. Oki Y, Fanale M, Westin JR, et al: 2013 ASH Annual Meeting. Abstract 252. Presented December 9, 2013.